Pleomorphic adenoma is a benign salivary gland tumor that exhibits wide cytomorphologic and architectural diversity. The tumor has the following 3 components:
- An epithelial cell component
- A myoepithelial cell component
- A stromal (mesenchymal) component
Epidemiology
Pleomorphic adenoma is the most common salivary gland tumor in both children and adults. In most series, it represents 45-75% of all salivary gland neoplasms; the annual incidence is approximately 2-3.5 cases per 100,000 population.
Pleomorphic adenoma occurs in individuals of all ages. However, it is most common in the third to sixth decades; the average age at presentation is between 43 and 46 years. Pleomorphic adenoma is seen more often in females than in males (2:1 ratio).
Pleomorphic adenoma occurs in individuals of all ages. However, it is most common in the third to sixth decades; the average age at presentation is between 43 and 46 years. Pleomorphic adenoma is seen more often in females than in males (2:1 ratio).
Location
Among the major salivary glands, the tail of the superficial lobe of the parotid salivary gland is the most common site of occurrence for pleomorphic adenoma (70-80% of cases), although this lesion can occur in any parotid location. The tumor is less commonly seen in the submandibular salivary gland (10%) and is seldom encountered in the sublingual gland (1%)With regard to the minor salivary glands (5-10% of cases), the palate (specifically, the junction of the soft and hard palates) and the lip are the most common sites for pleomorphic adenoma. Other sites of minor salivary gland involvement include the nose, the paranasal sinuses, and the larynx.
Rare or unusual sites of occurrence include ectopic salivary gland tissues (eg, in the mandible, neck lymph nodes, or axilla). A case has been reported of a pleomorphic adenoma presenting as a midline nodule in the isthmus of the thyroid in a 66-year-old man.
Clinical Features and Imaging
Pleomorphic adenoma usually presents as a slow-growing, painless mass, which may be present for many years. Symptoms and signs depend on the location.When the tumor occurs in the parotid gland, signs of facial nerve weakness are seldom encountered; however, if the tumor is large and has been neglected, facial nerve weakness is likely to arise as the result of malignant change. Pleomorphic adenoma in the deep lobe of the parotid gland may present as an oral retrotonsillar mass or parapharyngeal space tumor; indeed, tumors arising at this site are the source of the most common parapharyngeal space tumors. Rapid enlargement of a tumor nodule should raise concern about the development of malignant change.
Patients with minor salivary gland tumors may present with a variety of symptoms, depending on the site of the tumor; such symptoms include dysphagia, dyspnea, hoarseness, difficulty in chewing, and epistaxis.
Gross Findings
On gross examination, a pleomorphic adenoma is a single firm, mobile, well-circumscribed mass. Its color may vary from whitish-tan to gray to bluish, and its size may range from a few millimeters to quite large or even giant. Pleomorphic adenomas are irregularly shaped and have a bosselated surface.
Degenerative and cystic changes may be seen on sectioning. It is not unusual to observe evidence of focal or massive infarction. Recurrent tumors characteristically tend to present as multiple nodules of variable size.
Degenerative and cystic changes may be seen on sectioning. It is not unusual to observe evidence of focal or massive infarction. Recurrent tumors characteristically tend to present as multiple nodules of variable size.
Microscopic Findings
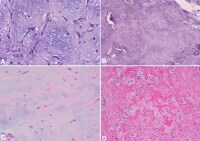
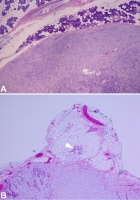
In the parotid gland, the tumor is usually surrounded by a fibrous capsule of variable thickness that may be focally deficient, especially in more mucoid tumors (see the image below). In minor salivary glands, no capsule is usually seen.
Capsule in pleomorphic adenoma. (A) Image shows pleomorphic adenoma with thin fibrous capsule separating tumor from surrounding normal parotid gland tissue. (B) Image shows pleomorphic adenoma with less well developed focally absent capsule. Note small satellite tumor nodule (arrow) protruding outside major tumor mass.
Microscopic satellite tumor nodules, pseudopodia, and capsular penetration may be seen beyond the capsule (see the image below). This may be the cause of recurrence of pleomorphic adenomas in cases that were treated with simple enucleation or in cases in which surgical resection was performed with inadequate surgical margins.
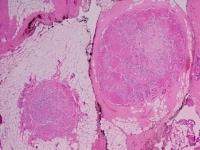
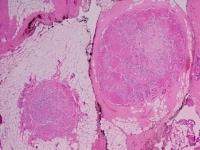
Recurrence of pleomorphic adenoma. Image shows recurrent pleomorphic adenoma with 2 microscopically benign–appearing nodules. Multinodular tumor pattern is characteristic in recurrent pleomorphic adenomas. The epithelial component consists of epithelial and myoepithelial cells with divergent growth patterns, including trabecular, tubular, solid, cystic, and papillary architecture.
Pure epithelial cells are mainly cuboidal. Cells that exhibit myoepithelial features[22, 23] may have plasmacytoid, epithelioid, spindle, oncocytic, or clear cell morphology.
In some studies, the most common myoepithelial cell type that was encountered displayed plasmacytoid cell morphology; the spindle cell type was the next most common type.[24] All cellular elements appear cytologically bland, with no significant mitotic activity.
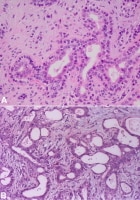
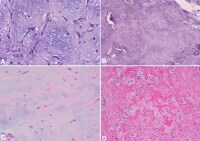
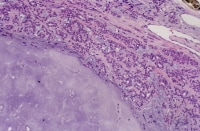
The ducts and tubules seen in pleomorphic adenomas usually exhibit a lining comprising 2 cell types—that is, an inner cuboidal epithelial cell layer and an outer myoepithelial cell layer (or layers) tend to merge into the surrounding stromal component, which also contains dispersed or grouped modified myoepithelial cells (see the image below). The cuboidal epithelial cells occasionally have a clear cytoplasm; the myoepithelial cell cytoplasm ranges from deeply eosinophilic to clear.
Pure epithelial cells are mainly cuboidal. Cells that exhibit myoepithelial features[22, 23] may have plasmacytoid, epithelioid, spindle, oncocytic, or clear cell morphology.
In some studies, the most common myoepithelial cell type that was encountered displayed plasmacytoid cell morphology; the spindle cell type was the next most common type.[24] All cellular elements appear cytologically bland, with no significant mitotic activity.
The ducts and tubules seen in pleomorphic adenomas usually exhibit a lining comprising 2 cell types—that is, an inner cuboidal epithelial cell layer and an outer myoepithelial cell layer (or layers) tend to merge into the surrounding stromal component, which also contains dispersed or grouped modified myoepithelial cells (see the image below). The cuboidal epithelial cells occasionally have a clear cytoplasm; the myoepithelial cell cytoplasm ranges from deeply eosinophilic to clear.
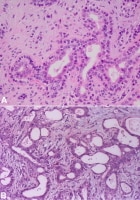
Cells in pleomorphic adenoma. (A) Tubule/duct formations in pleomorphic adenoma. Well-defined inner epithelial lining, consisting of cuboidal cells with eosinophilic cytoplasm, which can focally be clear, is surrounded by collar of 1 or more layers of myoepithelial cells with mostly clear cytoplasm. Stroma in between contains dispersed spindled and epithelioid myoepithelial cells. (B) Similar tubular arrangement is seen, but collar of myoepithelial cells is not as well defined. Stroma in between shows dispersed spindled myoepithelial cells. In both A and B, note bland nature of cells and absence of atypia.
In a limited biopsy specimen or in fine-needle aspiration (FNA), the characteristics seen in the ductal or tubular elements may cause the pleomorphic adenoma to be confused with other salivary gland tumors that have a similar architecture, such as adenoid cystic carcinoma and epithelial-myoepithelial carcinoma. In some cases, the tubules or ducts have a less well-defined surrounding myoepithelial layer.
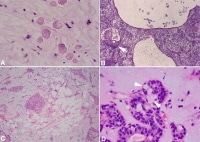
The stromal component is a product of the modified myoepithelial cells and may appear mucoid, myxoid, hyaline, chondroid, myxochondroid, or even osseous (see the image below).The stromal modified myoepithelial cell may undergo chondroid or osseous metaplasia.Chondroid areas represent true cartilage formation (containing type II collagen and keratin sulfate); this finding tends to be specific to pleomorphic adenoma and thus helps differentiate pleomorphic adenoma from other suspected salivary gland tumors.
The stromal component is a product of the modified myoepithelial cells and may appear mucoid, myxoid, hyaline, chondroid, myxochondroid, or even osseous (see the image below).The stromal modified myoepithelial cell may undergo chondroid or osseous metaplasia.Chondroid areas represent true cartilage formation (containing type II collagen and keratin sulfate); this finding tends to be specific to pleomorphic adenoma and thus helps differentiate pleomorphic adenoma from other suspected salivary gland tumors.
Different types of stroma in pleomorphic adenoma. (A) Myxoid stroma. Note dispersed spindle myoepithelial cells in stroma, some of which have stellate morphology. (B) Chondroid stroma. (C) Stroma with cartilage formation. (D) Hyalinized stroma. Some authors have found that a prominent hyalinized stroma is correlated with tumors that may have a propensity for malignant change. It is important to note that exuberant hyalinization may also be observed in other salivary gland tumors, especially adenoid cystic carcinoma.
When the cellular elements predominate, the result is an epithelial cell–rich or myoepithelial cell–rich (ie, cellular) pleomorphic adenoma; when the mesenchymal/stromal component predominates, the result is a stroma-rich pleomorphic adenoma (see the image below). A pleomorphic adenoma with an equal proportion of the 2 components is often referred to as a classic or mixed-type tumor.
When the cellular elements predominate, the result is an epithelial cell–rich or myoepithelial cell–rich (ie, cellular) pleomorphic adenoma; when the mesenchymal/stromal component predominates, the result is a stroma-rich pleomorphic adenoma (see the image below). A pleomorphic adenoma with an equal proportion of the 2 components is often referred to as a classic or mixed-type tumor.
Cellularity in pleomorphic adenoma. Image shows tumor with 2 contrasting regions. Visible in right upper part of image is cellular region with dense epithelial and myoepithelial cell component. In left lower part of image, dominant morphology is that of chondroid stroma, with only a few interspersed myoepithelial cells.
These differences in the cellular-stromal ratio do not appear to give rise to any clinical differences in tumor behavior. In many cases, however, different regions in the same tumor show striking variations in morphology and cellularity.
Pleomorphic adenoma occasionally exhibits unusual components, including sebaceous cells, mucous cells, squamous cells, oncocytic cells, serous acini, fibroadipose tissue,and crystal formations such as tyrosine or oxalate crystals (see the image below).
Pleomorphic adenoma occasionally exhibits unusual components, including sebaceous cells, mucous cells, squamous cells, oncocytic cells, serous acini, fibroadipose tissue,and crystal formations such as tyrosine or oxalate crystals (see the image below).
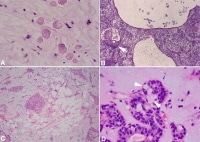
Unusual findings in pleomorphic adenoma. (A) Tyrosine crystals with characteristic rosette appearance. (B) Large cystic changes in pleomorphic adenoma that is rich in myoepithelial cells. Arrow indicates area of squamous cell metaplasia. (C) Foci of mature adipose tissue (fat) in the stroma. Note myoepithelial-rich stroma in background. (D) Areas of mucous signet–appearing cells (arrows) are present next to epithelial/myoepithelial formations.
The presence of mucous cells in pleomorphic adenoma, particularly in limited biopsy specimens, may prompt the examiner to consider entities such as mucoepidermoid carcinoma.[31, 32] However, the presence of other components (eg, stroma or myoepithelial cells) helps establish the correct interpretation.
Cystic changes are occasionally seen in pleomorphic adenoma. A large cyst may be present, or the tumor may be multicystic. However, such changes do not have an impact on the clinical course of the tumor.
Necrosis and increased mitosis are not commonly encountered in pleomorphic adenoma; when they do occur, a thorough search for evidence of malignant change is necessary. FNA or focal infarction may result in similar tumor changes, and this possibility should also be carefully considered. Other atypical findings, such as increased cellularity, focal atypia, pleomorphism, and capsular extension, should not be interpreted as indicating malignant change in the absence of other corroborating evidence.
The occasional presence of benign tumor fragments within vascular spaces in the tumor or in the immediate peritumoral vasculature is thought to result from perioperative manipulation of the tumor during surgical resection and should not be interpreted as indicating vascular invasion.
The presence of mucous cells in pleomorphic adenoma, particularly in limited biopsy specimens, may prompt the examiner to consider entities such as mucoepidermoid carcinoma.[31, 32] However, the presence of other components (eg, stroma or myoepithelial cells) helps establish the correct interpretation.
Cystic changes are occasionally seen in pleomorphic adenoma. A large cyst may be present, or the tumor may be multicystic. However, such changes do not have an impact on the clinical course of the tumor.
Necrosis and increased mitosis are not commonly encountered in pleomorphic adenoma; when they do occur, a thorough search for evidence of malignant change is necessary. FNA or focal infarction may result in similar tumor changes, and this possibility should also be carefully considered. Other atypical findings, such as increased cellularity, focal atypia, pleomorphism, and capsular extension, should not be interpreted as indicating malignant change in the absence of other corroborating evidence.
The occasional presence of benign tumor fragments within vascular spaces in the tumor or in the immediate peritumoral vasculature is thought to result from perioperative manipulation of the tumor during surgical resection and should not be interpreted as indicating vascular invasion.
Diagnosis
The diagnosis of salivary gland tumors utilize both tissue sampling and radiographic studies. Tissue sampling procedures include fine needle aspiration (FNA) and core needle biopsy (bigger needle comparing to FNA). Both of these procedures can be done in an outpatient setting. Diagnostic imaging techniques for salivary gland tumors include ultrasound, computer tomography (CT) and magnetic resonance imaging (MRI).Fine needle aspiration biopsy (FNA), operated in experienced hands, can determine whether the tumor is malignant in nature with sensitivity around 90%. FNA can also distinguish primary salivary tumor from metastatic disease.
Core needle biopsy can also be done in outpatient setting. It is more invasive but is more accurate compared to FNA with diagnostic accuracy greater than 97%.Furthermore, core needle biopsy allows more accurate histological typing of the tumor.
In terms of imaging studies, ultrasound can determine and characterize superficial parotid tumors. Certain types of salivary gland tumors have certain sonographic characteristics on ultrasound.Ultrasound is also frequently used to guide FNA or core needle biopsy.
CT allows direct, bilateral visualization of the salivary gland tumor and provides information about overall dimension and tissue invasion. CT is excellent for demonstrating bony invasion. MRI provides superior soft tissue delineation such as perineural invasion when compared to CT only.
Treatment
Overall, the mainstay of the treatment for salivary gland tumor is surgical resection. Needle biopsy is highly recommended prior to surgery to confirm the diagnosis. More detailed surgical technique and the support for additional adjuvant radiotherapy depends on whether the tumor is malignant or benign.Surgical treatment of parotid gland tumors is sometimes difficult, partly because of the anatomical relationship of the facial nerve and the parotid lodge, but also through the increased potential for postoperative relapse. Thus, detection of early stages of a tumor of the parotid gland is extremely important in terms of prognosis after surgery.
Generally, benign tumors of the parotid gland are treated with superficial(Patey's operation) or total parotidectomy with the latter being the more commonly practiced due to high incidence of recurrence.The facial nerve should be preserved whenever possible. The benign tumors of the submandibular gland is treated by simple excision with preservation of mandibular branch of the trigeminal nerve, the hypoglossal nerve, and the lingual nerve. Other benign tumors of minor salivary glands are treated similarly.
Malignant salivary tumors usually require wide local resection of the primary tumor. However, if complete resection cannot be achieved, adjuvant radiotherapy should be added to improve local control. This surgical treatment has many sequellae such as cranial nerve damage, Frey's syndrome, cosmetic problems, etc.
Usually about 44% of the patients have a complete histologic removal of the tumor and this refers to the most significant survival rate.
But the locoregional control rate for the carcinoma pleomorphic adenoma is only 66% in the 5-year duration of the recovery time making the recurrence of the disease invariably fatal, and even the 44% of the disease-related specific cases report to high rate of mortality accounting to 87%.
Net.

Comments
Post a Comment